|
Last updated: November 2022
Suggested citation: Greenhalgh, EM, Scollo, MM, & Pearce, M. 9.7 Explanations of socio-economic disparities in smoking. In Greenhalgh, EM, Scollo, MM and Winstanley, MH [editors]. Tobacco in Australia: Facts and issues. Melbourne: Cancer Council Victoria; 2022. Available from: http://www.tobaccoinaustralia.org.au/chapter-9-disadvantage/9-7-explanations-of-socioeconomic-disparities-in-s
|
'The relation between SES and smoking patterns is complex involving cumulative and multiple effects across the human life course, possibly extending from one generation to the next.' Gilman et al 2003 1 p807
Low socioeconomic status (SES) groups have substantially higher smoking rates than the overall population, both in Australia and internationally (see Section 9.1). Higher smoking rates among low-SES groups are associated with a web of interacting physiological, psychological, social, economic, commercial, and cultural factors,2 including:
- nicotine exposure in utero and during childhood3-6
- parental and peer relationships and modelling7-16
- lower achievement and satisfaction at school16-18 and lower educational attainment in adulthood19-21
- stress,22 , 23 mental illness,24-29 and substance use/dependence30
- a greater likelihood of belonging to a priority population among whom smoking is more common, such as Aboriginal and Torres Strait Islander peoples, people experiencing incarceration, or LGBTQI+ people
- social isolation31
- for minority groups, experiencing discrimination.32-34
- a lesser tendency to consider and value future outcomes35-38
- the endorsement of beliefs that minimise or discount the risks of smoking39
- workplaces40 and social circles41 that normalise smoking
- job loss42 and financial stress43
- a lower likelihood of working indoors44-46
- living in a disadvantaged neighbourhood47-50 or low-income housing51
- representations of smoking in popular culture52-55
- a history of targeted and intensive marketing56-60
- less success in maintaining cessation, despite being just as likely to make a quit attempt and to use cessation aids (see Section 9.8)
The above factors vary in importance in explaining socio-economic disparities at different developmental stages61 and at different stages in the tobacco addiction cycle.1 , 61 As with other aspects of social disadvantage, many factors driving tobacco-related disparities originate in childhood62-67 and accumulate throughout the individual’s life.64 , 68-70 It is also important to consider heterogeneity within groups, and that possessing multiple attributes that are associated with high smoking prevalence (for example, belonging to a priority group and having a lower education level) may interact and further increase a person’s risk of smoking.71 , 72
While a wealth of information is available on associations between social disadvantage and tobacco use,73-75 understanding the causal mechanisms underlying these associations is more challenging.76 Nonetheless, recent studies suggest that some of these factors can causally impact a person’s risk of smoking. For example, a large study in the UK found that more years of education leads to reduced likelihood of smoking uptake, and reduced heaviness of smoking and greater likelihood of quitting among smokers.19 Another UK study suggests that the relationship between disadvantage and smoking uptake can largely be explained by parental modelling of smoking. That is, reducing disadvantaged children’s exposure to smoking may largely reduce future disparities in tobacco use.77
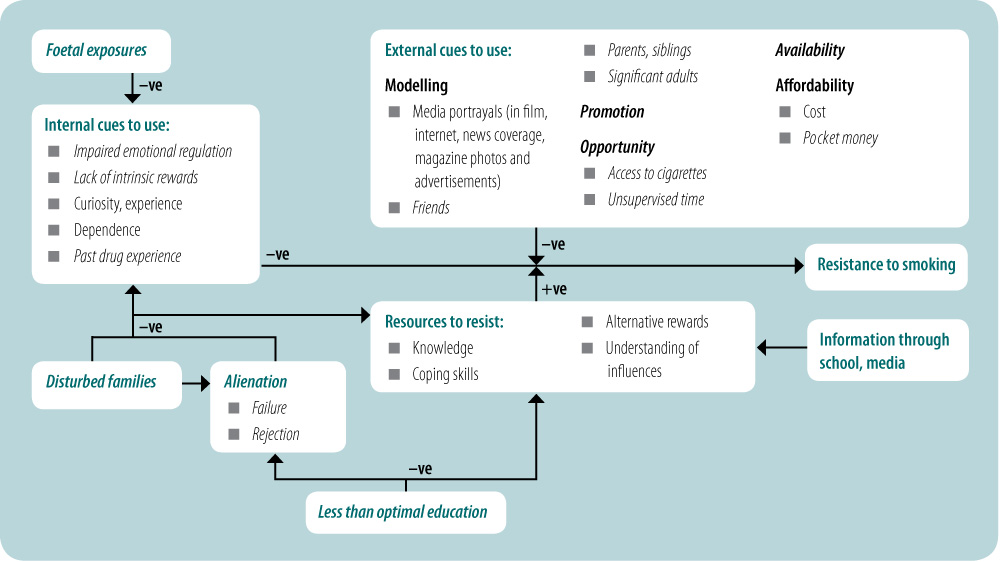
Figures 9.7.1 and 9.7.2 show how a variety of physiological, psychological and sociological factors may maintain socio-economic disparities in smoking uptake and smoking cessation.
See InDepth 9A for a detailed discussion of smoking prevalence, the role of smoking in health and social inequalities, and cessation interventions tailored and targeted for: people living in regional and remote areas of Australia; culturally and linguistically diverse groups; people with substance use and mental disorders; people experiencing homelessness; people experiencing incarceration; lesbian, gay, bisexual, trans, queer and intersex (LGBTQI+) people; military personnel and veterans; and single parents
Relevant news and research
For recent news items and research on this topic, click
here.
( Last updated March 2024)
References
1. Gilman SE, Abrams DB, and Buka SL. Socioeconomic status over the life course and stages of cigarette use: initiation, regular use, and cessation. Journal of Epidemiology and Community Health, 2003; 57(10):802–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/14573586
2. Siahpush M. Why is lone motherhood so strongly associated with smoking in Australia? Australian and New Zealand Journal of Public Health, 2004; 28(1):37–42. Available from: https://europepmc.org/article/MED/15108745
3. Macleod J, Hickman M, Bowen E, Alati R, Tilling K, et al. Parental drug use, early adversities, later childhood problems and children's use of tobacco and alcohol at age 10: birth cohort study. Addiction, 2008; 103(10):1731–43. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18705686
4. Graham H, Hawkins SS, and Law C. Lifecourse influences on women's smoking before, during and after pregnancy. Social Science & Medicine, 2010; 70(4):582–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19932931
5. Hanson MD and Chen E. Socioeconomic status and health behaviors in adolescence: a review of the literature. Journal of Behavioral Medicine, 2007; 30(3):263–85. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17514418
6. Hayatbakhsh M, Mamun A, Najman J, O'Callaghan M, Bor W, et al. Early childhood predictors of early substance use and substance use disorders: prospective study. Australian and New Zealand Journal of Psychiatry, 2008; 42(8):720–31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18622780
7. Richter M, Vereecken CA, Boyce W, Maes L, Gabhainn SN, et al. Parental occupation, family affluence and adolescent health behaviour in 28 countries. International Journal of Public Health, 2009; 54(4):203–12. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19347249
8. Rainio S, Rimpelä A, Luukkaala T, and Rimpelä M. Evolution of the association between parental and child smoking in Finland between 1977 and 2005. Preventive Medicine, 2008; 46(6):565–71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18289657
9. Paul SL, Blizzard L, Patton GC, Dwyer T, and Venn A. Parental smoking and smoking experimentation in childhood increase the risk of being a smoker 20 years later: the Childhood Determinants of Adult Health Study. Addiction, 2008; 103(5):846–53. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18412765
10. Audrain-McGovern J, Rodriguez D, Tercyak KP, Neuner G, and Moss HB. The impact of self-control indices on peer smoking and adolescent smoking progression. J Pediatr Psychol, 2006; 31(2):139–51. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16467314
11. Melchior M, Chastang JF, Mackinnon D, Galera C, and Fombonne E. The intergenerational transmission of tobacco smoking--the role of parents' long-term smoking trajectories. Drug and Alcohol Dependence, 2010; 107(2-3):257–60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20004064
12. Brook JS, Morojele NK, Brook DW, Zhang C, and Whiteman M. Personal, interpersonal, and cultural predictors of stages of cigarette smoking among adolescents in Johannesburg, South Africa. Tobacco Control, 2006; 15 Suppl 1(suppl. 1):i48–53. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16723676
13. Fraga S, Sousa S, Ramos E, Dias I, and Barros H. Social representations of smoking behaviour in 13-year-old adolescents. Rev Port Pneumol, 2011; 17(1):27–31. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21251481
14. Kim MJ, Fleming CB, and Catalano RF. Individual and social influences on progression to daily smoking during adolescence. Pediatrics, 2009; 124(3):895–902. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19706575
15. DiNapoli P. Early initiation of tobacco use in adolescent girls: key sociostructural influences. Applied Nursing Research : ANR, 2009; 22(2):126–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19427575
16. Pedersen W and Soest TV. How is low parental socioeconomic status associated with future smoking and nicotine dependence in offspring? A population-based longitudinal 13-year follow-up. Scand J Public Health, 2017; 45(1):16–24. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27913689
17. Moor I, Rathmann K, Lenzi M, Pfortner TK, Nagelhout GE, et al. Socioeconomic inequalities in adolescent smoking across 35 countries: a multilevel analysis of the role of family, school and peers. European Journal of Public Health, 2015; 25(3):457–63. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25713016
18. Fergusson DM, Horwood LJ, Boden JM, and Jenkin G. Childhood social disadvantage and smoking in adulthood: results of a 25-year longitudinal study. Addiction, 2007; 102(3):475–82. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17298656
19. Gage SH, Bowden J, Davey Smith G, and Munafo MR. Investigating causality in associations between education and smoking: a two-sample Mendelian randomization study. Int J Epidemiol, 2018; 47(4):1131–40. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29961807
20. Gugushvili A, Zhao Y, and Bukodi E. Intergenerational educational mobility and smoking: a study of 20 European countries using diagonal reference models. Public Health, 2020; 181:94–101. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31981813
21. Villanti AC, Johnson AL, and Rath JM. Beyond education and income: Identifying novel socioeconomic correlates of cigarette use in U.S. young adults. Preventive Medicine, 2017; 104:63–70. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28647547
22. Hobkirk AL, Krebs NM, and Muscat JE. Income as a moderator of psychological stress and nicotine dependence among adult smokers. Addictive Behaviors, 2018; 84:215–23. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29729584
23. Jahnel T, Ferguson SG, Shiffman S, and Schuz B. Daily stress as link between disadvantage and smoking: an ecological momentary assessment study. BMC Public Health, 2019; 19(1):1284. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31606051
24. Strong DR, Cameron A, Feuer S, Cohn A, Abrantes AM, et al. Single versus recurrent depression history: differentiating risk factors among current US smokers. Drug and Alcohol Dependence, 2010; 109(1-3):90–5. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20074868
25. Trosclair A and Dube SR. Smoking among adults reporting lifetime depression, anxiety, anxiety with depression, and major depressive episode, United States, 2005-2006. Addictive Behaviors, 2010; 35(5):438–43. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20079577
26. Khaled SM, Bulloch A, Exner DV, and Patten SB. Cigarette smoking, stages of change, and major depression in the Canadian population. Can J Psychiatry, 2009; 54(3):204–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19321025
27. Cougle JR, Zvolensky MJ, Fitch KE, and Sachs-Ericsson N. The role of comorbidity in explaining the associations between anxiety disorders and smoking. Nicotine & Tobacco Research, 2010; 12(4):355–64. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20156885
28. Goodwin RD, Wall MM, Garey L, Zvolensky MJ, Dierker L, et al. Depression among current, former, and never smokers from 2005 to 2013: The hidden role of disparities in depression in the ongoing tobacco epidemic. Drug and Alcohol Dependence, 2017; 173:191–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28209289
29. Martinez SA, Beebe LA, Thompson DM, Wagener TL, Terrell DR, et al. A structural equation modeling approach to understanding pathways that connect socioeconomic status and smoking. PLoS One, 2018; 13(2):e0192451. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29408939
30. Higgins ST, Kurti AN, Redner R, White TJ, Keith DR, et al. Co-occurring risk factors for current cigarette smoking in a U.S. nationally representative sample. Preventive Medicine, 2016; 92:110–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26902875
31. Shareck M, Kestens Y, and Frohlich KL. Moving beyond the residential neighborhood to explore social inequalities in exposure to area-level disadvantage: Results from the Interdisciplinary Study on Inequalities in Smoking. Social Science & Medicine, 2014; 108:106–14. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24632055
32. Parker LJ, Kinlock BL, Chisolm D, Furr-Holden D, and Thorpe RJ, Jr. Association Between Any Major Discrimination and Current Cigarette Smoking Among Adult African American Men. Substance Use and Misuse, 2016; 51(12):1593–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27484877
33. Agunwamba AA, Kawachi I, Williams DR, Finney Rutten LJ, Wilson PM, et al. Mental Health, Racial Discrimination, and Tobacco Use Differences Across Rural-Urban California. Journal of Rural Health, 2017; 33(2):180–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27074968
34. Pearson JL, Waa A, Siddiqi K, Edwards R, Nez Henderson P, et al. Naming Racism, not Race, as a Determinant of Tobacco-Related Health Disparities. Nicotine & Tobacco Research, 2021; 23(6):885–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/33822185
35. Khwaja A, Silverman D, and Sloan F. Time preference, time discounting, and smoking decisions. J Health Econ, 2007; 26(5):927–49. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17574694
36. VanderVeen JW, Cohen LM, Cukrowicz KC, and Trotter DR. The role of impulsivity on smoking maintenance. Nicotine & Tobacco Research, 2008; 10(8):1397–404. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18686188
37. Businelle MS, McVay MA, Kendzor D, and Copeland A. A comparison of delay discounting among smokers, substance abusers, and non-dependent controls. Drug and Alcohol Dependence, 2010; 112(3):247–50. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20696538
38. Fields S, Leraas K, Collins C, and Reynolds B. Delay discounting as a mediator of the relationship between perceived stress and cigarette smoking status in adolescents. Behavioural Pharmacology, 2009; 20(5–6):455–60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19730366
39. Guillaumier A, Bonevski B, Paul C, D'Este C, Twyman L, et al. Self-Exempting Beliefs and Intention to Quit Smoking within a Socially Disadvantaged Australian Sample of Smokers. International Journal of Environmental Research and Public Health, 2016; 13(1). Available from: https://www.ncbi.nlm.nih.gov/pubmed/26761022
40. Sorensen G, Emmons K, Stoddard AM, Linnan L, and Avrunin J. Do Social Influences Contribute to Occupational Differences in Quitting Smoking and Attitudes toward Quitting? American Journal of Health Promotion, 2002; 16(3):135–41. Available from: http://ahp.sagepub.com/content/16/3/135.abstract
41. Hitchman SC, Fong GT, Zanna MP, Thrasher JF, Chung-Hall J, et al. Socioeconomic status and smokers' number of smoking friends: findings from the International Tobacco Control (ITC) Four Country Survey. Drug and Alcohol Dependence, 2014; 143:158–66. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25156228
42. Golden SD and Perreira KM. Losing jobs and lighting up: Employment experiences and smoking in the Great Recession. Social Science & Medicine, 2015; 138:110–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26079992
43. Twyman L, Bonevski B, Paul C, Bryant J, West R, et al. Factors Associated With Concurrent Tobacco Smoking and Heavy Alcohol Consumption Within a Socioeconomically Disadvantaged Australian Sample. Substance Use and Misuse, 2016; 51(4):459–70. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26942661
44. Smith DR. Tobacco smoking by occupation in Australia and the United States: a review of national surveys conducted between 1970 and 2005. Industrial Health 2008; 46:77–89. Available from: http://www.jstage.jst.go.jp/article/indhealth/46/1/46_77/_article
45. Smith DR and Leggat PA. Tobacco smoking by occupation in Australia: results from the 2004 to 2005 National Health Survey. J Occup Environ Med, 2007; 49(4):437–45. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17426527
46. Germain D, McCarthy M, and Durkin S. Smoking bans in Victorian workplaces: reduced disparities in exposure to secondhand smoke, 1998 to 2007. CBRC Research Paper Series No. 35, Melbourne, Australia: Centre for Behavioural Research in Cancer, Cancer Council Victoria, 2008.
47. Cambron C, Kosterman R, and Hawkins JD. Neighborhood Poverty Increases Risk for Cigarette Smoking From Age 30 to 39. Annals of Behavioral Medicine, 2019; 53(9):858–64. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30395158
48. Caraballo RS, Rice KL, Neff LJ, and Garrett BE. Social and Physical Environmental Characteristics Associated With Adult Current Cigarette Smoking. Preventing Chronic Disease, 2019; 16:E71. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31172916
49. Siahpush M and Borland R. Sociodemographic variations in smoking status among Australians aged 18 years and over: multivariate results from the 1995 National Health Survey. Australian and New Zealand Journal of Public Health, 2001; 25(2):438–42. Available from: https://pubmed.ncbi.nlm.nih.gov/11688624/
50. Rachele JN, Wood L, Nathan A, Giskes K, and Turrell G. Neighbourhood disadvantage and smoking: Examining the role of neighbourhood-level psychosocial characteristics. Health Place, 2016; 40:98–105. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27228312
51. Jackson SE, Smith C, Cheeseman H, West R, and Brown J. Finding smoking hot-spots: a cross-sectional survey of smoking patterns by housing tenure in England. Addiction, 2019; 114(5):889–95. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30597650
52. Martyn CN. Smoking in british popular culture 1800-2000. British Medical Journal, 2000; 321(7257):389. Available from: https://www.ncbi.nlm.nih.gov/pubmed/10926605
53. Krupka LR, Vener AM, and Richmond G. Tobacco advertising in gender-oriented popular magazines. J Drug Educ, 1990; 20(1):15–29. Available from: https://www.ncbi.nlm.nih.gov/pubmed/2348303
54. Healton CG, Watson-Stryker ES, Allen JA, Vallone DM, Messeri PA, et al. Televised movie trailers: undermining restrictions on advertising tobacco to youth. Arch Pediatr Adolesc Med, 2006; 160(9):885–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16953010
55. Soulos G and Sanders S. Promoting tobacco to the young in the age of advertising bans. N S W Public Health Bull, 2004; 15(5-6):104–6. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15543244
56. John R, Cheney MK, and Azad MR. Point-of-sale marketing of tobacco products: taking advantage of the socially disadvantaged? Journal of Health Care for the Poor and Underserved, 2009; 20(2):489–506. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19395844
57. Apollonio DE and Malone RE. Marketing to the marginalised: tobacco industry targeting of the homeless and mentally ill. Tobacco Control, 2005; 14(6):409–15. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16319365
58. Siahpush M, Jones PR, Singh GK, Timsina LR, and Martin J. The association of tobacco marketing with median income and racial/ethnic characteristics of neighbourhoods in Omaha, Nebraska. Tobacco Control, 2010; 19(3):256–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20395407
59. Siahpush M, Jones PR, Singh GK, Timsina LR, and Martin J. Association of availability of tobacco products with socio-economic and racial/ethnic characteristics of neighbourhoods. Public Health, 2010; 124(9):525–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20723950
60. Brown-Johnson CG, England LJ, Glantz SA, and Ling PM. Tobacco industry marketing to low socioeconomic status women in the U.S.A. Tobacco Control, 2014; 23(e2):e139–46. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24449249
61. Moolchan ET, Fagan P, Fernander AF, Velicer WF, Hayward MD, et al. Addressing tobacco-related health disparities. Addiction, 2007; 102 Suppl 2(suppl. 2):30–42. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17850612
62. Brunner E, Shipley M, Blane D, and al e. When does cardiovasular risk start? Past and present socioeconomic circumstances and risk factors in adulthood. Journal of Epidemiology and Community Health, 1999; 53(12):757–64. Available from: http://jech.bmj.com/cgi/reprint/53/12/757
63. Power C, Graham H, Due P, Hallqvist J, Joung I, et al. The contribution of childhood and adult socioeconomic position to adult obesity and smoking behaviour: an international comparison. Int J Epidemiol, 2005; 34(2):335–44. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15659473
64. Galobardes B, Lynch J, and Smith DG. Childhood socioeconomic circumstances and cause-specific mortality in adulthood: systematic review and interpretation. Epidemiologic Reviews, 2004; 26(1):7–21. Available from: http://epirev.oxfordjournals.org/cgi/content/full/26/1/7
65. Harville EW, Boynton-Jarrett R, Power C, and Hypponen E. Childhood hardship, maternal smoking, and birth outcomes: a prospective cohort study. Arch Pediatr Adolesc Med, 2010; 164(6):533–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20530303
66. Evans GW and Kutcher R. Loosening the link between childhood poverty and adolescent smoking and obesity: the protective effects of social capital. Psychol Sci, 2011; 22(1):3–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21106889
67. Topitzes J, Mersky JP, and Reynolds AJ. Child maltreatment and adult cigarette smoking: a long-term developmental model. Journal of Pediatric Psychology, 2010; 35(5):484-98. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19995869
68. Gilman SE, Abrams DB, and Buka SL. Socioeconomic status over the life course and stages of cigarette use: initiation, regular use, and cessation. Journal of Epidemiolgy and Community Health, 2003; 57(10):802–8. Available from: http://jech.bmj.com/cgi/content/abstract/57/10/802
69. Case A, Lubotsky D, and Paxson C. Economic Status and Health in Childhood: The Origins of the Gradient. Am Econ Rev, 2002; 92(5):1308–34. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29058397
70. Chen E, Martin AD, and Matthews KA. Socioeconomic status and health: do gradients differ within childhood and adolescence? Social Science & Medicine 2006; 62(9):2161–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16213644
71. Sheffer CE, Williams JM, Erwin DO, Smith PH, Carl E, et al. Tobacco-Related Disparities Viewed Through the Lens of Intersectionality. Nicotine & Tobacco Research, 2022; 24(2):285–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/34555170
72. Tan ASL, Hinds JT, Smith PH, Antin T, Lee JP, et al. Incorporating intersectionality as a framework for equity-minded tobacco control research - A call for collective action toward a paradigm shift. Nicotine & Tobacco Research, 2022. Available from: https://www.ncbi.nlm.nih.gov/pubmed/35439321
73. Fagan P, Moolchan ET, Lawrence D, Fernander A, and Ponder PK. Identifying health disparities across the tobacco continuum. Addiction, 2007; 102 Suppl 2(suppl. 2):5–29. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17850611
74. Harwood GA, Salsberry P, Ferketich AK, and Wewers ME. Cigarette smoking, socioeconomic status, and psychosocial factors: examining a conceptual framework. Public Health Nurs, 2007; 24(4):361–71. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17553026
75. Giordano G and Lindstrom M. The impact of social capital on changes in smoking behaviour: a longitudinal cohort study. European Journal of Public Health, 2011; 21(3):347-54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20570962
76. Birch S. Commentary: Social inequalities in health, social epidemiology and social value. Int J Epidemiol, 2001; 30(2):294–6. Available from: https://www.ncbi.nlm.nih.gov/pubmed/11369730
77. Taylor-Robinson DC, Wickham S, Campbell M, Robinson J, Pearce A, et al. Are social inequalities in early childhood smoking initiation explained by exposure to adult smoking? Findings from the UK Millennium Cohort Study. PLoS One, 2017; 12(6):e0178633. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28575096