A strategy sometimes adopted by people who are trying to minimise their risk of adverse health outcomes from smoking is to attempt to smoke only occasionally. 1 , 2 Many people who have been regular smokers try to reduce their risk of harm by cutting down on the number of cigarettes smoked each day. 3 In 2019, about 300,000 Australians smoked at least once a week but not every day. Another 300,000 smoked at least once a month but not every week. 4 In 2019, more than half of all current Australian smokers aged 14 years and over reported attempting over the previous year to reduce the amount of tobacco/number of cigarettes they smoked each day—14% unsuccessfully and 39% managing to cut down to at least some extent. 4
Greater perceptions that smoking is harmful are associated with a greater likelihood of being a non-daily smoker, 5 with non-daily smokers generally perceiving their smoking as posing fewer health harms than daily smoking. 6 The logic of minimising or cutting down smoking as a strategy for minimising or reducing harm is supported by a large body of research showing that the association between smoking and many diseases becomes stronger with more cigarettes smoked each day (i.e., a dose—response relationship). 7 , 8 Despite this relationship, evidence from prospective cohort studies does not support low intensity (“light”) smoking, 9-13 or occasional (“social”) smoking 13 as an effective way to avoid risk from tobacco smoking. Neither does it support cutting down as an effective method to substantially reduce overall risk of death. 13-15 ,16
As outlined in Section 3.36.1 , even very low levels of exposure can cause cancer or create changes in the cardiovascular system: there is no safe level of smoking. 7 , 17 A number of studies have found elevated overall risk and risk of death from smoking-related diseases in light daily smokers compared to never smokers 9 , 18-20 and even in occasional, non-daily smokers. 13 The findings of the largest and most recent studies 11-13 and most comprehensive reviews 9 are listed below in sections 3.36.2 and 3.36.3. Moving from heavy to moderate and moderate to light levels of smoking does not substantially reduce risk, 14 , 15 particularly for coronary heart disease and stroke 13 , 16 —see 3.36.4 . The main advantage of smokers cutting down the number of cigarettes per day may be as a step that makes it easier to quit completely 21 , 22 —see 3.36.5 .
3.36.1 Biological mechanisms for low-rate smoking posing substantial major health risks
One explanation for lack of substantial risk reduction after reduction in smoking is compensation: smokers who cut down on number of cigarettes per day (CPD) tend to take more and deeper puffs from each cigarette, and smoke more of it. 23 , 24 The same phenomenon has been observed with waterpipe smoking. 25 In turn, there is a much smaller proportional reduction in intake of nicotine, tar, and other toxins than the amount of cutting down might predict. 26 In the US, Black people who smoke have higher disease risk than White smokers, despite smoking fewer cigarettes per day, and this has been attributed to the intensity with which each cigarette is smoked. 27 Studies measuring biomarkers of the dangerous substances in tobacco smoke (see Section 12.5.6) find that, compared to quitting completely, smokers who cut down still have relatively high levels of biomarkers of oxidative stress (an imbalance of free radicals and antioxidants in the body) such as glutathione 28 and other metabolites such as thiocyanate, 29 TNE-2, NNAL, NNN, 2-Fluorene, HPMA, CYMA, and MHB3. 30
Another reason why low-rate smoking is not substantially less risky, is that the relationship between exposure to tobacco smoke and damage caused is not linear. 7 , 8 , 31-33
Because there is no safe level of exposure to carcinogens, cancer can develop even with very low levels of exposure, 34 including 1–3 cigarettes per day 35 and non-daily smoking. 36 A recent study in the US found that non-daily smokers had substantially higher concentrations of urinary NNAL than non-smokers, with concentrations in the range that is associated with an increased risk of lung cancer. 37 Duration of smoking has a greater effect on risk than smoking intensity. 31 It is more dangerous to smoke a small number of cigarettes for many years than it is to smoke the same number of cigarettes over a shorter period. 8 , 35 , 38-40
With coronary heart disease, the non-linear relationship is even more striking. 41 While many of the processes that drive the development of coronary heart disease do result in more risk with greater consumption, there is one notable exception. Aggregation of platelet cells in the blood—known as the ‘sticky blood phenomenon’, which increases the risk of blood clots and heart attacks and stroke—is elevated at only one cigarette per day and does not worsen substantially with higher cigarette consumption. That is, the maximal effect occurs at a very low levels of smoking. 42 Platelet aggregation occurs not only at low levels of smoking but also among those exposed to second-hand smoke. 42 (highlighted in USSG 2010, 7 Chapter 6, p 358).
3.36.2 Risks associated with low-rate daily smoking
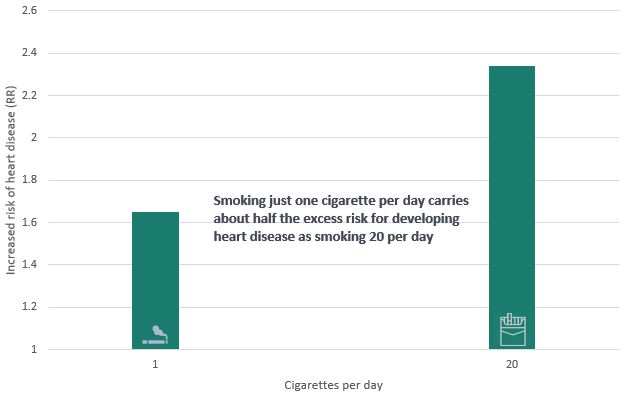
A 2018 meta-analysis of 141 cohort studies summarised in 55 scientific papers reported that, on average, smoking only one cigarette per day carries a risk of developing coronary heart disease and stroke much greater than expected: around half that for people who smoke 20 per day—that is, 10/20 th rather than the 1/20 th that might be expected. 9 This strongly suggests that there is no safe level of smoking for cardiovascular disease. The authors estimated that among a group of 100 middle-aged people, a 20-a-day cigarette habit would cause an extra seven heart attacks or strokes. But if those people drastically cut back to one a day, smoking would still cause three additional heart attacks. 9
Figure 3.36.1 Risk of heart disease among those that smoke 1 cigarette per day compared to those that smoke 20 cigarettes per day
Since the 2018 meta-analysis, a prospective study of 188,167 cardiovascular disease (CVD)- and cancer-free individuals aged 45 years and older from the NSW general population (the ’45 and Up’ study) revealed similar findings. 11 The researchers compared the probability of hospitalisation with or without mortality from CVD between current and past versus never smokers, and whether this varies by intensity and recency of smoking. During an average of 7.2 years follow-up fatal and non-fatal major CVD events occurred, including 4548 (crude rate 3.2/1000 person-years) acute myocardial infarction (AMI; or heart attack), 3991 (2.8) cerebrovascular disease, 3874 (2.7) heart failure and 2311 (1.6) peripheral arterial disease (PAD) events. CVD risks were elevated at almost all levels of current smoking intensity and increased with smoking intensity. While risks of CVD mortality were largest for those who smoked 25 or more cigarettes per day (HR=4.90 (3.79–6.34)), they were still considerable for those who smoked 4–6 cigarettes per day (1.92 (1.11–3.32)). The same study has shown that even light smoking (1–5 cigarettes per day) increased the incidence of lung cancer by more than nine times compared with never smokers (HR 9.22, 5.14-16.55). It found that by age 80, an estimated 7.7% of current smokers who smoke 1–5 cigarettes per day will develop lung cancer. 43
A very large US study published in 2020 similarly found surprisingly high levels of risk for those smoking five or fewer cigarettes per day. 12 Data were from 13 waves of the National Health Interview Survey (1997 to 2009) that were linked to death records through December 31, 2011. During a median follow-up of 8.2 years, 34,862 participants died, of which 8,415 were from cancer, 9,031 from CVD, and 2,040 from respiratory disease. Compared with never-smokers, participants who smoked 1–2 or 3–5 cigarettes per day were at higher risk of all-cause mortality even after adjustment for demographic variables, lifestyle factors and physician-diagnosis of chronic disease. The risks were similar for the two levels of smoking—1–2 cigarettes per day (HR = 1.94, 1.73–2.16) and 3–5 cigarettes per day (HR = 1.99, 1.83–2.17). The associations were strongest for deaths from respiratory disease, followed by cancer and CVD. For example, among those smoking 1–2 cigarettes per day, risk of death was 9.75 times greater (HR; 95%CI 6.15–15.46), 2.28 (1.84–2.84) times greater, and 1.93 (1.58–2.36) times greater, respectively, for these three cause-specific mortalities.
An analysis of data from the US Current Population Survey published in 2020 similarly found that compared with those who smoked 11–20 cigarettes per day, mortality risks were only slightly lower among those that smoke 3–10 cigarettes per day, and appeared to be similar to daily smokers who smoked >1–2 cigarettes. Even daily smokers who smoked just one cigarette per day had substantially higher mortality risks than never smokers. 13 A large prospective study in Mexico has also examined mortality risk among daily smokers who smoked fewer than ten cigarettes per day, and found that low-intensity daily smoking was associated with increased mortality. Compared with never smokers, light daily smokers had elevated risks of death from respiratory cancers, chronic obstructive pulmonary disease, and gastrointestinal and cardiac diseases. 44
Another very large study, this time in Japan, found increased mortality risks for those who smoked 1–2 cigarettes per day, which increased alongside additional cigarettes per day. In men, mortality risks for 1–2 cigarettes per day were higher than never smokers for smoking-related cancer, lung cancer, circulatory disease and subarachnoid haemorrhage. Among women who smoked 1–5 cigarettes per day, higher mortality risks were observed for lung cancer, ischaemic heart disease, cerebrovascular disease, subarachnoid haemorrhage, and respiratory disease. Ex-smokers had lower mortality risks than current smokers, including those who smoked 10 or fewer cigarettes per day, and these lower risks were particularly pronounced among those who quit at younger ages. 45
Taken together, these studies show the substantial benefits of quitting for heart and general health, with even very light smoking increasing a person’s risk of angina, heart attack or stroke.
3.36.3 Risks associated with non-daily smoking
In the US since the 2010s, several very large cohort studies linked to national morbidity and mortality data bases have increasingly allowed researchers to study the effects of infrequent smoking over long periods of time.
One large study of 39,555 participants in the US Million Heart studies found no difference in blood pressure and cholesterol levels between ‘social’ smokers and current smokers: rates of hypertension and elevated cholesterol were significantly higher among both groups compared to never smokers. 46
Another large US cohort study published in 2018 tracked death and disease up to 2011 among 70,913 adults who were interviewed in the US National Health Interview Surveys in 1991, 1992 and 1995. 47 The long-term non-daily smokers smoked a median of 15 days and 50 cigarettes a month, compared with a median of 600 cigarettes per month among daily smokers. As expected, daily smokers had the highest mortality risks (HR=2.50, 95% CI=2.35, 2.66) and shorter survival (10 years less) than never smokers. However, mortality risks were also surprisingly high among those who only smoked occasionally. Compared with never smokers, lifelong non-daily smokers (i.e. people who smoked but had never smoked daily) had a 72% higher mortality risk (HR=1.72 95% CI=1.36, 2.18) including for cancer, cardiovascular disease, and respiratory disease mortalities. Compared to never smokers, higher mortality risks were observed among lifelong non-daily smokers who reported smoking:
- 11–30 cigarettes per month (HR=1.34, 95% CI=0.81, 2.20);
- 31–60 cigarettes per month (HR=2.02, 95% CI=1.17, 3.29); and
- >60 cigarettes per month (HR=1.74, 95% CI=1.12, 2.72).
Median life-expectancy was about five years shorter for lifelong non-daily smokers than for never smokers. The researchers concluded that although the mortality risks of non-daily smokers are lower than those of daily smokers, they are still substantial. 47
An even larger study published by the same researchers in 2020 examined the records of more than 500,000 American ever-smokers who had completed a Tobacco Use Supplement administered as part of the US Census Bureau’s Current Population Survey between 1992–93 and 2010–11. 13 Records were linked to the US National Death Index.
As with the earlier study, the median number of cigarettes smoked per month was 600—10–20 cigarettes per day—for daily cigarette smokers and 40 cigarettes per month for lifelong non-daily smokers. Once again, both current daily smokers (HR= 2.32; 95% CI, 2.25–2.38) and lifelong non-daily smokers (HR= 1.82; 95% CI, 1.65–2.01) had higher all-cause mortality risks than never smokers. Mortality risks were elevated even among lifelong non-daily smokers who smoked as few as 6 to 10 cigarettes per month.
3.36.4 Effects of moving from heavier to lighter rates of smoking
A 2020 meta-analysis examined the effects of moving from heavy (≥15–20 cigarettes per day (CPD)) to moderate (10–19 CPD) or light (<10 CPD) levels of smoking on lung cancer, other smoking related cancers, stroke, coronary heart disease (defined as myocardial infarction and ischemic heart disease combined) and cardiovascular disease (defined as stroke and coronary heart disease. It also examined the effects of reducing smoking by a third, or by half, compared with continuing to smoke heavily. 16
As shown in figure 3.36.2 (as indicated by the darker bars), while reducing smoking decreased the risk of lung cancer, results for other health outcomes were mixed and often showed no benefit of cutting down.
Figure 3.36.2 Relative risk for each smoking reduction category on health outcomes. Darker bars indicate significantly decreased risk; error bars show 95% CIs.
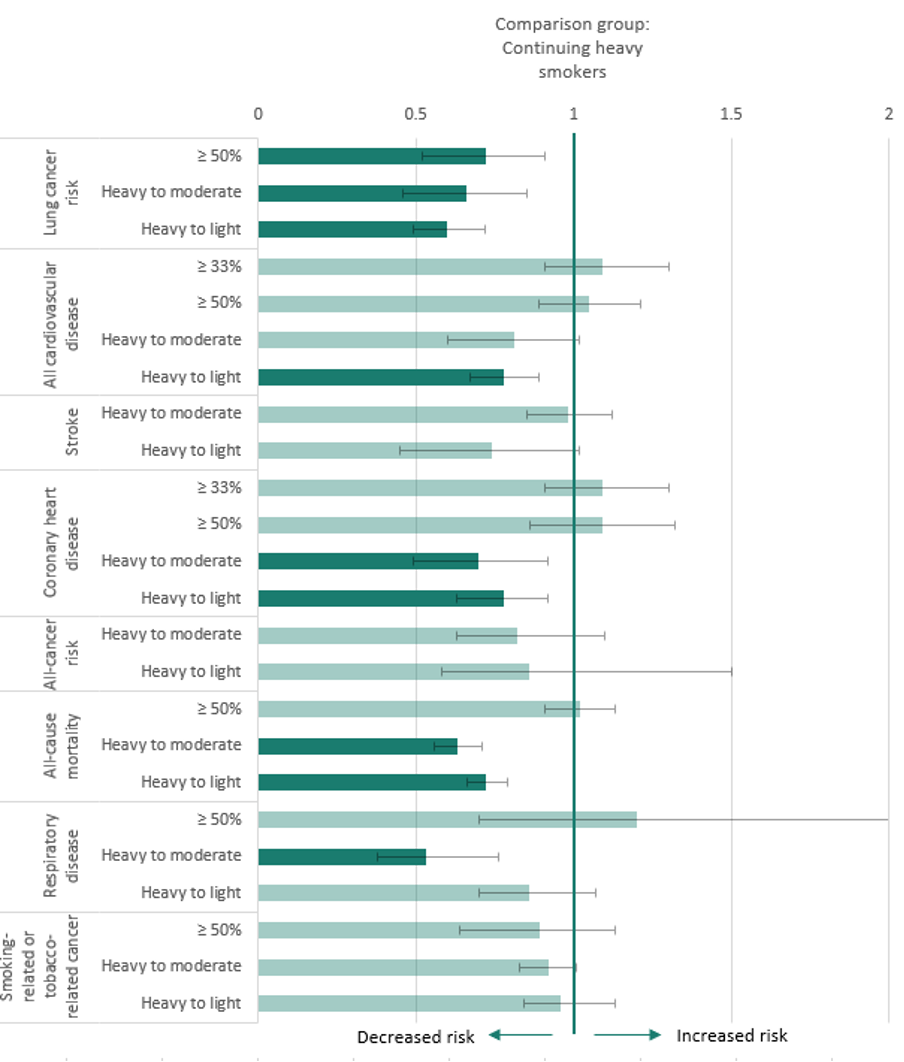
The researchers concluded that although smoking reduction may decrease lung cancer risks by about one-quarter to one-third, the size of risk reduction is not proportional to the reduction in consumption, and the absolute magnitude of lung cancer risk remains high even among those who cut down substantially. Results showed no benefits of cutting down for decreasing risk of other cancers or stroke, and mixed findings for other health outcomes. Complete cessation remains the most effective approach for cancer and CVD prevention.
As discussed in 3.36.3 above, the large US Current Population Survey cohort survey did find some reduction in risk for former daily smokers who became non-daily smokers. 13
Relative to never smokers, mortality risks for a smoking-related cancer were
- 2.16 times (95%CI, 1.64–2.86) higher among lifetime non-daily smokers,
- 3.65 times (95%CI, 3.11–4.27) higher among non-daily previous daily smokers and
- 4.88 times (95%CI, 4.57–5.22) higher among continuing daily smokers. 13
Non-daily smokers who previously smoked every day had lower overall mortality risks than daily smokers, particularly if they reduced their smoking at least ten years ago; compared with never smokers, their risk of dying early was 1.7 times higher (95% CI, 1.56–1.92). However, this risk was still much higher than for daily smokers who quit completely. Among former daily smokers who had quit for ten years or more, the risk of dying early was 1.2 times higher (95% CI 1.15–1.22) than never smokers.
Figure 3.36.3 Risk of dying early compared to someone who has never smoked
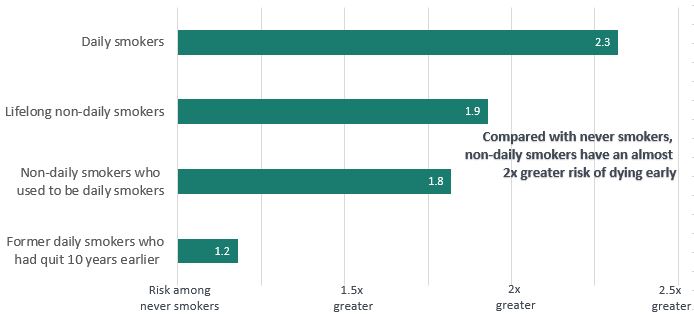
The authors conclude that although reducing smoking from daily to non-daily was associated with decreased mortality risk, cessation was associated with far greater benefit.
A large Korean study published in 2021 examined the effects of quitting smoking, reducing smoking by 50% or more, reducing smoking by 20–50%, sustaining the same level of smoking, or increasing smoking on a person’s risk of cardiovascular disease (stroke and heart attack). Compared with those who sustained their cigarette consumption, quitting was associated with a reduced risk of both stroke (aHR 0.77, 95% CI 0.74–0.81) and heart attack (aHR 0.74, 95% CI 0.70–0.78). However, there was no reduction in risk for those who reduced smoking, even among those who reduced by more than 50%. Additional analysis showed that those who quit but then relapsed had 42–69% increased risk of heart attack and stroke compared to sustained quitters, highlighting both the importance of quitting and staying quit for reducing the risk of cardiovascular disease. 48
3.36.5 Cutting down as a step towards quitting
The primary benefit of cutting down seems to be its role as a step toward quitting. 19 , 21 , 49-51 — see Section 7.6.2 for a detailed discussion of ‘cutting down to quit’ as a cessation strategy.
The existing epidemiological evidence on cutting down providing limited health benefit (as summarised above) is generally in the context of no additional source of nicotine, such as NRT or e-cigarettes. Obtaining nicotine from an alternative source may reduce some of the compensatory smoking behaviour that would otherwise limit the benefit from cutting down. Studies of smokers cutting down while using NRT have found that while blood nicotine levels generally remain stable or slightly higher, carbon monoxide readings decreased. 52-54 This has led some to advocate concomitant use of NRT while smoking as a harm reduction strategy. 55 Further, NRT-assisted smoking reduction is associated with increased cessation rates among smokers unmotivated to quit. 56 However, data on the health risks/benefits of long-term dual use (i.e., for those who of NRT and other alternative nicotine delivery products and cigarettes are lacking.
The fact remains that even low-intensity smoking—even occasional non-daily smoking—is associated with substantially elevated risks of death among ever-smokers. Complete cessation of tobacco smoking is the only way of reducing these risks.
Relevant news and research
A comprehensive compilation of news items and research published on this topic
Read more on this topic
References
1. Li X, Loukas A, and Perry CL. Very light smoking and alternative tobacco use among college students. Addictive Behaviors, 2018; 81:22–5. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29421346
2. Amrock SM and Weitzman M. Adolescents' perceptions of light and intermittent smoking in the United States. Pediatrics, 2015; 135(2):246–54. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25583910
3. Britton J and Bogdanovica I. Electronic cigarettes: a report commissioned by Public Health England. 2014. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/311887/Ecigarettes_report.pdf
4. Australian Institute of Health and Welfare. Data tables: National Drug Strategy Household Survey 2019 - 2. Tobacco smoking chapter, Supplementary data tables. Canberra: AIHW, 2020. Available from: https://www.aihw.gov.au/reports/illicit-use-of-drugs/national-drug-strategy-household-survey-2019/data
5. Land SR, Baker L, Bachand J, Twesten J, Kaufman AR, et al. Associations of Daily Versus Nondaily Smoking, Tobacco-Related Risk Perception, and Cancer Diagnosis Among Adults in the Population Assessment of Tobacco and Health (PATH) Study. Nicotine & Tobacco Research, 2022; 24(10):1540–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/35245943
6. Schane RE, Glantz SA, and Ling PM. Nondaily and social smoking: an increasingly prevalent pattern. Archives of Internal Medicine, 2009; 169(19):1742–4. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19858429
7. US Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease. A report of the US Surgeon General, Atlanta, Georgia: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53017/
8. International Agency for Research on Cancer, Personal habits and indoor combustions. IARC Monographs Vol. Volume 100 E A review of human carcinogens.Lyon, France: IARC; 2012. Available from: https://www.ncbi.nlm.nih.gov/books/NBK304391/.
9. Hackshaw A, Morris JK, Boniface S, Tang JL, and Milenkovic D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. British Medical Journal, 2018; 360:j5855. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29367388
10. Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, et al. Association of Long-term, Low-Intensity Smoking With All-Cause and Cause-Specific Mortality in the National Institutes of Health-AARP Diet and Health Study. JAMA Internal Medicine, 2017; 177(1):87–95. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27918784
11. Banks E, Joshy G, Korda RJ, Stavreski B, Soga K, et al. Tobacco smoking and risk of 36 cardiovascular disease subtypes: fatal and non-fatal outcomes in a large prospective Australian study. BMC Medicine, 2019; 17(1):128. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31266500
12. Qin W, Magnussen CG, Li S, Steffen LM, Xi B, et al. Light Cigarette Smoking Increases Risk of All-Cause and Cause-Specific Mortality: Findings from the NHIS Cohort Study. International Journal of Environmental Research and Public Health, 2020; 17(14). Available from: https://www.ncbi.nlm.nih.gov/pubmed/32679883
13. Inoue-Choi M, Christensen CH, Rostron BL, Cosgrove CM, Reyes-Guzman C, et al. Dose-Response Association of Low-Intensity and Nondaily Smoking With Mortality in the United States. JAMA Netw Open, 2020; 3(6):e206436. Available from: https://www.ncbi.nlm.nih.gov/pubmed/32492162
14. Pisinger C and Godtfredsen NS. Is there a health benefit of reduced tobacco consumption? A systematic review. Nicotine & Tobacco Research, 2007; 9(6):631–46. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17558820
15. Inoue-Choi M, Hartge P, Park Y, Abnet CC, and Freedman ND. Association Between Reductions of Number of Cigarettes Smoked per Day and Mortality Among Older Adults in the United States. American Journal of Epidemiology, 2019; 188(2):363–71. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30299454
16. Chang JT, Anic GM, Rostron BL, Tanwar M, and Chang CM. Cigarette Smoking Reduction and Health Risks: A Systematic Review and Meta-analysis. Nicotine & Tobacco Research, 2021; 23(4):635–42. Available from: https://www.ncbi.nlm.nih.gov/pubmed/32803250
17. Katsi V, Maragkoudakis S, Ioakeimidis N, Marketou M, Parthenakis F, et al. The cardiovascular burden of light smoking. Arch Med Sci Atheroscler Dis, 2021; 6:e48–e56. Available from: https://www.ncbi.nlm.nih.gov/pubmed/34027214
18. Bjartveit K and Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tobacco Control, 2005; 14(5):315–20. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16183982
19. Hart C, Gruer L, and Bauld L. Does smoking reduction in midlife reduce mortality risk? Results of 2 long-term prospective cohort studies of men and women in Scotland. American Journal of Epidemiology, 2013; 178(5):770–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23825165
20. Tverdal A and Bjartveit K. Health consequences of reduced daily cigarette consumption. Tobacco Control, 2006; 15(6):472–80. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17130377
21. Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, et al. 'Cut down to quit' with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis. Health Technology Assessment, 2008; 12(2):1–135. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18093448
22. Lindson N, Klemperer E, Hong B, Ordonez-Mena JM, and Aveyard P. Smoking reduction interventions for smoking cessation. Cochrane Database of Systematic Reviews, 2019; 9(9):CD013183. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31565800
23. Shiffman S, Dunbar MS, and Benowitz NL. A comparison of nicotine biomarkers and smoking patterns in daily and nondaily smokers. Cancer Epidemiology, Biomarkers & Prevention, 2014; 23(7):1264–72. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24740202
24. Krebs NM, Chen A, Zhu J, Sun D, Liao J, et al. Comparison of Puff Volume With Cigarettes per Day in Predicting Nicotine Uptake Among Daily Smokers. American Journal of Epidemiology, 2016; 184(1):48–57. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27313218
25. Brinkman MC, Kim H, Buehler SS, Adetona AM, Gordon SM, et al. Evidence of compensation among waterpipe smokers using harm reduction components. Tobacco Control, 2020; 29(1):15–23. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30377243
26. McNeill A. Harm reduction. Review. British Medical Journal, 2004; 328(7444):885–7. Available from: http://www.bmj.com/cgi/content/full/328/7444/885
27. Ho JTK, Tyndale RF, Baker TB, Amos CI, Chiu A, et al. Racial disparities in intensity of smoke exposure and nicotine intake among low-dependence smokers. Drug and Alcohol Dependence, 2021; 221:108641. Available from: https://www.ncbi.nlm.nih.gov/pubmed/33652379
28. Mons U, Muscat JE, Modesto J, Richie JP, Jr., and Brenner H. Effect of smoking reduction and cessation on the plasma levels of the oxidative stress biomarker glutathione--Post-hoc analysis of data from a smoking cessation trial. Free Radic Biol Med, 2016; 91:172–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26708755
29. Theophilus EH, Coggins CR, Chen P, Schmidt E, and Borgerding MF. Magnitudes of biomarker reductions in response to controlled reductions in cigarettes smoked per day: a one-week clinical confinement study. Regulatory Toxicology and Pharmacology, 2015; 71(2):225–34. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25572415
30. Rostron BL, Corey CG, Chang JT, van Bemmel DM, Miller ME, et al. Changes in Cigarettes per Day and Biomarkers of Exposure Among US Adult Smokers in the Population Assessment of Tobacco and Health Study Waves 1 and 2 (2013-2015). Nicotine & Tobacco Research, 2020; 22(10):1780–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/32221599
31. International Agency for Research on Cancer. Reversal of risk after quitting smoking. IARC handbooks of cancer prevention, tobacco control, 11 Vol. 11.Lyon, France: IARC, 2007. Available from: http://apps.who.int/bookorders/anglais/detart1.jsp?sesslan=1&codlan=1&codcol=76&codcch=22
32. Popell CA, Burnett RT, Krewski D, Jerrett M, Shi Y, et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke shape of the exposure-response relationship. Circulation, 2009; 120(11):941–48. Available from: http://circ.ahajournals.org/content/120/11/941.short
33. Schane RE, Ling PM, and Glantz SA. Health effects of light and intermittent smoking: a review. Circulation, 2010; 121(13):1518–22. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20368531
34. International Agency for Research on Cancer. Tobacco smoking. IARC Monographs on the evaluation of the carniogenic risk of chemicals to humans, 11 Vol 38.Lyon, France: IARC, 1986. Available from: https://publications.iarc.fr/56
35. Berthiller J, Straif K, Agudo A, Ahrens W, Bezerra Dos Santos A, et al. Low frequency of cigarette smoking and the risk of head and neck cancer in the INHANCE consortium pooled analysis. Int J Epidemiol, 2016; 45(3):835–45. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26228584
36. Bjerregaard BK, Raaschou-Nielsen O, Sorensen M, Frederiksen K, Tjonneland A, et al. The effect of occasional smoking on smoking-related cancers: in the European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Causes Control, 2006; 17(10):1305–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17111263
37. Gutierrez-Torres DS, Wang L, Blount BC, Xia B, Sosnoff CS, et al. Concentrations of Cotinine and 4-(Methylnitrosamino)-1-(3-Pyridyl)-1-Butanol (NNAL) in U.S. Non-Daily Cigarette Smokers. Cancer Epidemiology, Biomarkers & Prevention, 2021; 30(6):1165–74. Available from: https://www.ncbi.nlm.nih.gov/pubmed/33737303
38. Doll R and Peto R. Cigarette smoking and bronchial carcinoma: dose and time relationships among regular smokers and lifelong non-smokers. J Epidemiol Community Health (1978), 1978; 32(4):303–13. Available from: https://www.ncbi.nlm.nih.gov/pubmed/744822
39. Flanders WD, Lally CA, Zhu BP, Henley SJ, and Thun MJ. Lung cancer mortality in relation to age, duration of smoking, and daily cigarette consumption: results from Cancer Prevention Study II. Cancer Res, 2003; 63(19):6556–62. Available from: https://www.ncbi.nlm.nih.gov/pubmed/14559851
40. Lubin JH and Caporaso NE. Cigarette smoking and lung cancer: modeling total exposure and intensity. Cancer Epidemiology, Biomarkers & Prevention, 2006; 15(3):517–23. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16537710
41. Luoto R, Uutela A, and Puska P. Occasional smoking increases total and cardiovascular mortality among men. Nicotine & Tobacco Research, 2000; 2(2):133–9. Available from: https://www.ncbi.nlm.nih.gov/pubmed/11072451
42. Law MR and Wald NJ. Environmental tobacco smoke and ischemic heart disease. Prog Cardiovasc Dis, 2003; 46(1):31–8. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12920699
43. Weber MF, Sarich PEA, Vaneckova P, Wade S, Egger S, et al. Cancer incidence and cancer death in relation to tobacco smoking in a population-based Australian cohort study. International Journal of Cancer, 2021; 149(5):1076–88. Available from: https://www.ncbi.nlm.nih.gov/pubmed/34015143
44. Thomson B, Tapia-Conyer R, Lacey B, Lewington S, Ramirez-Reyes R, et al. Low-intensity daily smoking and cause-specific mortality in Mexico: prospective study of 150 000 adults. Int J Epidemiol, 2021; 50(3):955–64. Available from: https://www.ncbi.nlm.nih.gov/pubmed/33659992
45. Inoue-Choi M, Freedman ND, Saito E, Tanaka S, Hirabayashi M, et al. Low-intensity cigarette smoking and mortality risks: a pooled analysis of prospective cohort studies in Japan. Int J Epidemiol, 2022; 51(4):1276–90. Available from: https://www.ncbi.nlm.nih.gov/pubmed/34718588
46. Gawlik KS, Melnyk BM, and Tan A. An Epidemiological Study of Population Health Reveals Social Smoking as a Major Cardiovascular Risk Factor. American Journal of Health Promotion, 2018; 32(5):1221–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28464696
47. Inoue-Choi M, McNeel TS, Hartge P, Caporaso NE, Graubard BI, et al. Non-Daily Cigarette Smokers: Mortality Risks in the U.S. American Journal of Preventive Medicine, 2019; 56(1):27–37. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30454906
48. Jeong SM, Jeon KH, Shin DW, Han K, Kim D, et al. Smoking cessation, but not reduction, reduces cardiovascular disease incidence. European Heart Journal, 2021; 42(40):4141–53. Available from: https://www.ncbi.nlm.nih.gov/pubmed/34431997
49. Hyland A, Levy DT, Rezaishiraz H, Hughes JR, Bauer JE, et al. Reduction in amount smoked predicts future cessation. Psychology of Addictive Behaviors, 2005; 19(2):221–5. Available from: https://www.ncbi.nlm.nih.gov/pubmed/16011395
50. Klemperer EM, Hughes JR, Callas PW, and Solomon LJ. A Mediation Analysis of Motivational, Reduction, and Usual Care Interventions for Smokers Who Are Not Ready to Quit. Nicotine & Tobacco Research, 2017; 19(8):916–21. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28182218
51. Klemperer EM, Hughes JR, and Callas PW. Increasing Quit Attempts by Transitioning to Very Low Nicotine Content Cigarettes Versus Reducing Number of Cigarettes Per Day: A Secondary Analysis of an Exploratory Randomized Trial. Nicotine & Tobacco Research, 2019; 21(Suppl 1):S81–S7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31867643
52. Dalack GW and Meador-Woodruff JH. Acute feasibility and safety of a smoking reduction strategy for smokers with schizophrenia. Nicotine & Tobacco Research, 1999; 1(1):53–7. Available from: https://www.ncbi.nlm.nih.gov/pubmed/11072388
53. Bolliger CT, Zellweger JP, Danielsson T, van Biljon X, Robidou A, et al. Smoking reduction with oral nicotine inhalers: double blind, randomised clinical trial of efficacy and safety. British Medical Journal, 2000; 321(7257):329–33. Available from: https://www.ncbi.nlm.nih.gov/pubmed/10926587
54. Fagerstrom KO, Tejding R, Westin A, and Lunell E. Aiding reduction of smoking with nicotine replacement medications: hope for the recalcitrant smoker? Tobacco Control, 1997; 6(4):311–6. Available from: https://www.ncbi.nlm.nih.gov/pubmed/9583629
55. Bittoun R, Barone M, Mendelsohn CP, Elcombe EL, and Glozier N. Promoting positive attitudes of tobacco-dependent mental health patients towards NRT-supported harm reduction and smoking cessation. Australian and New Zealand Journal of Psychiatry, 2014; 48(10):954–6. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24907132
56. Begh R, Lindson-Hawley N, and Aveyard P. Does reduced smoking if you can't stop make any difference? BMC Medicine, 2015; 13:257. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26456865